What is continuous glucose monitoring?
Continuous glucose monitoring automatically tracks blood glucose levels, also called blood sugar, throughout the day and night. You can see your glucose level anytime at a glance. You can also review how your glucose changes over a few hours or days to see trends. Seeing glucose levels in real time can help you make more informed decisions throughout the day about how to balance your food, physical activity, and medicines.
How does a continuous glucose monitor (CGM) work?
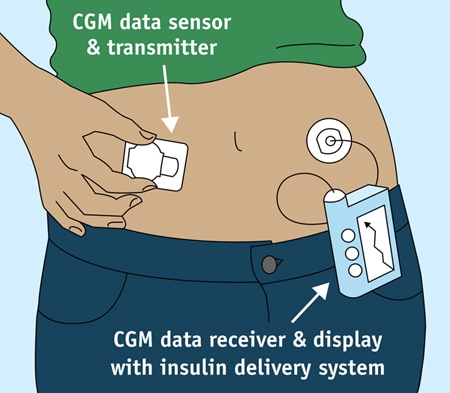
A CGM works through a tiny sensor inserted under your skin, usually on your belly or arm. The sensor measures your interstitial glucose level, which is the glucose found in the fluid between the cells. The sensor tests glucose every few minutes. A transmitter wirelessly sends the information to a monitor.
The monitor may be part of an insulin pump or a separate device, which you might carry in a pocket or purse. Some CGMs send information directly to a smartphone or tablet. Several models are available and are listed in the American Diabetes Association’s product guide External link.
Special Features of a CGM
CGMs are always on and recording glucose levels—whether you’re showering, working, exercising, or sleeping. Many CGMs have special features that work with information from your glucose readings:
- An alarm can sound when your glucose level goes too low or too high.
- You can note your meals, physical activity, and medicines in a CGM device, too, alongside your glucose levels.
- You can download data to a computer or smart device to more easily see your glucose trends.
Some models can send information right away to a second person’s smartphone—perhaps a parent, partner, or caregiver. For example, if a child’s glucose drops dangerously low overnight, the CGM could be set to wake a parent in the next room.
Currently, one CGM model is approved for treatment decisions, the Dexcom G5 Mobile. That means you can make changes to your diabetes care plan based on CGM results alone. With other models, you must first confirm a CGM reading with a finger-stick blood glucose test before you take insulin or treat hypoglycemia.
Special Requirements Needed to Use a CGM
Twice a day, you may need to check the CGM itself. You’ll test a drop of blood on a standard glucose meter. The glucose reading should be similar on both devices.
You’ll also need to replace the CGM sensor every 3 to 7 days, depending on the model.
For safety it’s important to take action when a CGM alarm sounds about high or low blood glucose. You should follow your treatment plan to bring your glucose into the target range, or get help.

Who can use a CGM?
Most people who use CGMs have type 1 diabetes. Research is underway to learn how CGMs might help people with type 2 diabetes.
CGMs are approved for use by adults and children with a doctor’s prescription. Some models may be used for children as young as age 2. Your doctor may recommend a CGM if you or your child:
- are on intensive insulin therapy, also called tight blood sugar control
- have hypoglycemia unawareness
- often have high or low blood glucose
Your doctor may suggest using a CGM system all the time or only for a few days to help adjust your diabetes care plan.
What are the benefits of a CGM?
Compared with a standard blood glucose meter, using a CGM system can help you
- better manage your glucose levels every day
- have fewer low blood glucose emergencies
- need fewer finger sticks
A graphic on the CGM screen shows whether your glucose is rising or dropping—and how quickly—so you can choose the best way to reach your target glucose level.
Over time, good management of glucose greatly helps people with diabetes stay healthy and prevent complications of the disease. People who gain the largest benefit from a CGM are those who use it every day or nearly every day.
What are the limits of a CGM?
Researchers are working to make CGMs more accurate and easier to use. But you still need a finger-stick glucose test twice a day to check the accuracy of your CGM against a standard blood glucose meter.
With most CGM models, you can’t yet rely on the CGM alone to make treatment decisions. For example, before changing your insulin dose, you must first confirm a CGM reading by doing a finger-stick glucose test.
A CGM system is more expensive than using a standard glucose meter. Check with your health insurance plan or Medicare NIH external link to see whether the costs will be covered.

What is an artificial pancreas?
A CGM is one part of the “artificial pancreas” systems that are beginning to reach people with diabetes.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has played an important role in developing artificial pancreas technology. An artificial pancreas replaces manual blood glucose testing and the use of insulin shots. A single system monitors blood glucose levels around the clock and provides insulin or both insulin and a second hormone, glucagon, automatically. The system can also be monitored remotely, for example by parents or medical staff.
In 2016, the U.S. Food and Drug Administration approved a type of artificial pancreas system called a hybrid closed-loop system External link. This system tests your glucose level every 5 minutes throughout the day and night through a CGM, and automatically gives you the right amount of basal insulin, a long-acting insulin, through a separate insulin pump. You will still need to test your blood with a glucose meter a few times a day. And you’ll manually adjust the amount of insulin the pump delivers at mealtimes and when you need a correction dose.
The hybrid closed-loop system may free you from some of the daily tasks needed to keep your blood glucose stable—or help you sleep through the night without the need to wake and test your glucose or take medicine. Talk with your health care provider about whether this system might be right for you.
The NIDDK has funded – and continues to fund – several important studies on different types of artificial pancreas devices to better help people with type 1 diabetes manage their disease. The devices may also help people with type 2 diabetes and gestational diabetes.